Cervix cancer elimination: Time to scale up awareness, screening and vaccination
By Dr. R. Sankaranarayanan
Cervical cancer is a type of cancer that occurs in the covering cells of the lower part of the uterus called cervix that connect both to the vagina and the body of the uterus. It is a very common cancer among poor women in low- and middle-income countries (LMICs). World Health Organization’s (WHO) specialised cancer agency called the International Agency for Research on Cancer (IARC) located in Lyons, documents and publishes the most authentic detailed estimation of occurrence of new cases and cancer deaths as well as prevalence of cancer cases (new cancer cases plus surviving cases) for the world, different WHO region, continents, income categories and different countries. WHO-IARC estimates that 604,000 new cases and 342,000 cervical cancer deaths occurred in 2020 globally of which more than 95% occur in LMICs. Cervical cancer accounted for 124,000 new cases and 77,000 deaths in 2020 in India. Worldwide cervical cancer is the fourth most common cancer preceded by breast, large bowel and lung among women and in India the second most common cancer in women.
What causes cervical cancer?
Cervix cancer is caused by persistent infection of the female lower genital tract (cervix, vagina, vulva) by one of the 14 types of the Human Papillomavirus (HPV). It is the most common, ubiquitous viral infection of the lower genital tract.
Among the HPV types implicated in cervical cancer causation, HPV 16 and HPV 18 account for 70-80% of cervical cancer cases. All most all women get infected with one or more of the HPV after sexual debut; fortunately HPV infection clears by itself in more than 90% of the infected women. Thus when exposed to HPV infection, the body’s protective immune system clears these viruses in most women thereby preventing the virus from doing harm.
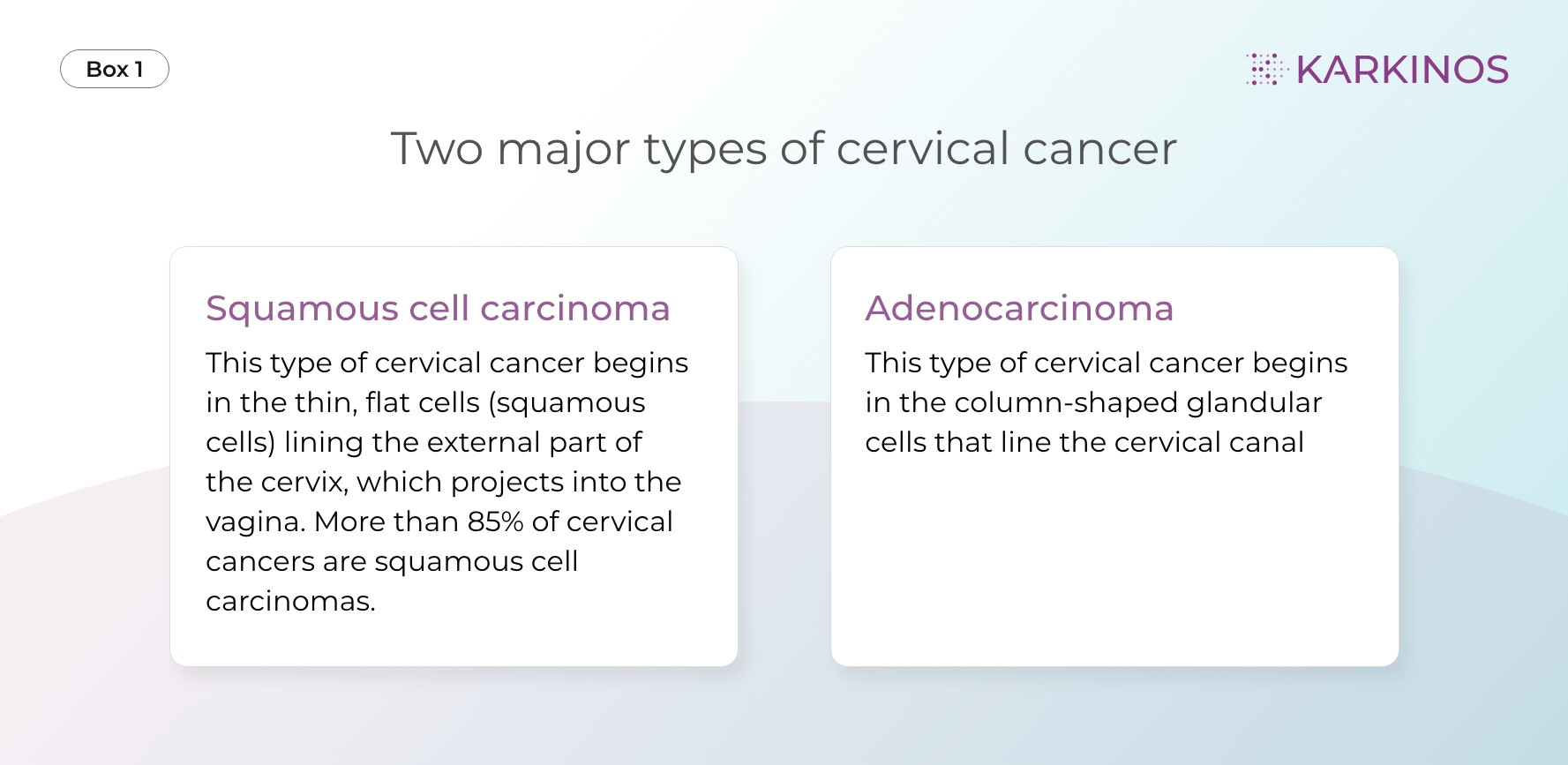
In a small percentage of people, however, the virus survives for years, contributing to the process that causes some cervical cells to become cancer cells that may progress to cervical cancer precursor lesions called cervical intraepithelial neoplasia grades 2 or 3 (CIN 2 or CIN 3) or adenocarcinoma in-situ (AIS) and frank cervical cancer (refer Box 1). HPV 16 and HPV 18 infections persist much more than other HPV types.
Although HPV infection is very common, and most women with the virus never develop cancer which indicates other factors such as poor nutrition, and other environmental or lifestyle factors also determine whether women with HPV infection develop cervical cancer. Most HPV infections clear up on their own and most pre-cancerous lesions resolve spontaneously, nevertheless there is a risk for all women that HPV infection may become chronic and cause pre-cancerous lesions that might progress to invasive cervical cancer. It takes 15 to 20 years for cervical cancer to develop in apparently healthy women whereas it might take only 5 to 10 years in women with weakened immune systems, such as those with untreated human immunodeficiency virus (HIV) infection. Women living with HIV are six times more likely to get cervical cancer compared to women without HIV infection
Prevention of cervical cancer
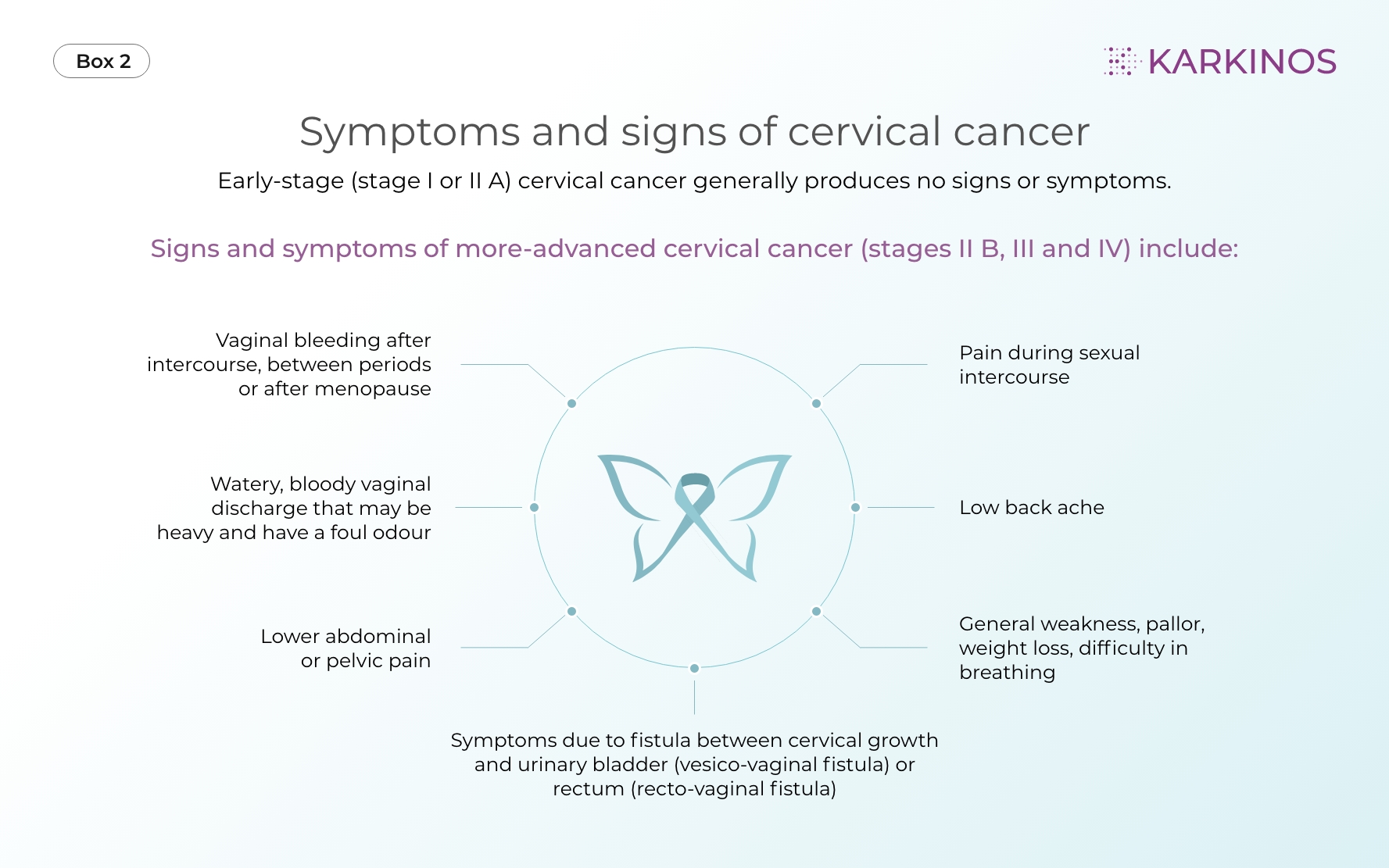
Cervical cancer is an eminently preventable disease and amenable for elimination, provided women are vaccinated against HPV infection and screened with one of the screening tests such as HPV testing, Pap smear or visual inspection with acetic acid (VIA) for early detection of precancerous lesions such as CIN and AIS at appropriate ages and their effective treatment. Even invasive cervical cancer in symptomatic women (Box 2) can be detected in early clinical stages such as stages I A, I B and IIA which can be effectively treated with surgery or radiotherapy with cure rates ranging between 85-95%. Thus early diagnosis of symptomatic cervical cancer cases and adequate treatment may substantially avoid cervical cancer deaths. If the above interventions are provided to a large number of women in the community, the incidence of cervical cancer can be prevented substantially.
Elimination of cervical cancer
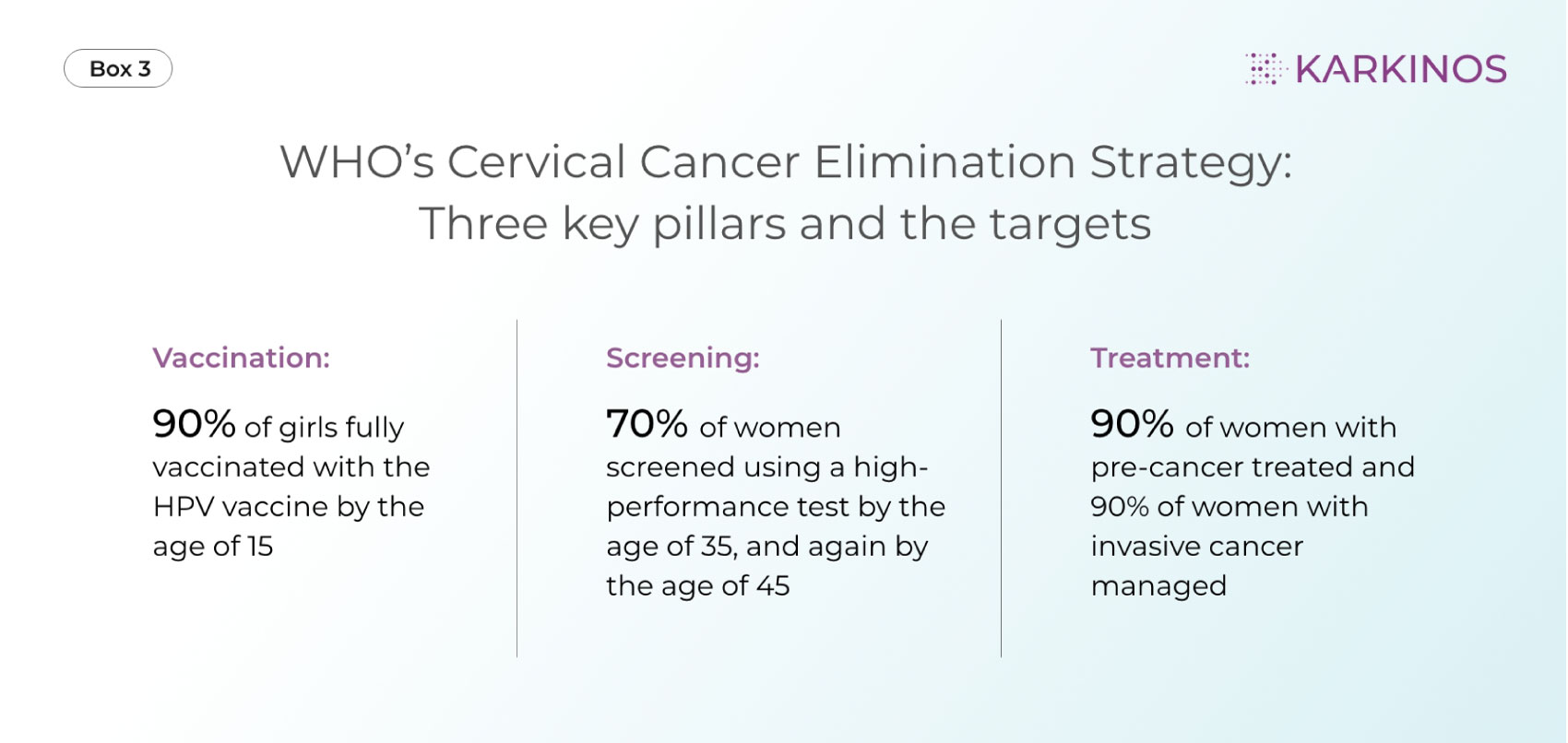
Taking note of the elimination of potential cervical cancer and the much neglected area of women’s health vis-à-vis maternal mortality, the WHO Director-General in May 2018 announced a global call for action to eliminate cervical cancer and called for all stakeholders to unite behind this common goal. In August 2020 the World Health Assembly adopted an ambitious and inclusive Global Strategy for Cervical Cancer Elimination to guide the elimination of cervical cancer as a public health problem. To eliminate cervical cancer, all countries must reach and maintain an incidence rate of below four per 100 000 women. Achieving that goal rests on three key pillars of vaccination, screening and early diagnosis of cancer linked with treatment and their corresponding targets (Box 3). Each country should meet the 90-70-90 targets by 2030 to get on the path to eliminate cervical cancer within the next century.
Is it possible to eliminate cervical cancer?
It is possible to reach and maintain an incidence rate of 4 per 100,000 women or less by vaccinating 90% of the girls with two doses of human papillomavirus (HPV) vaccination separated by 6-12 month interval before they reach 15 years; and screening 70% of adult women aged 30 years and above using a highly accurate test such as testing for HPV infection and treating adequately screen positive women found with precancerous lesions (stage 0).
In addition, early diagnosis and adequate treatment of cervical cancer with surgery or chemoradiotherapy can cure a large proportion of early stage (stages I and II A) cervical cancer patients. It is critical that more than 90% of women detected with cervical precancerous lesions or cancer should receive adequate treatment well in time. For maximum impact, the 90%-70%-90% targets must be implemented simultaneously.
In countries such as Australia which has made substantial progress in implementing the 90%-70%-90% strategy, cervical cancer is estimated to be eliminated between 2028 and 2035. However, to keep, cervical cancer eliminated Australia should continue with the 90%-70%-90% strategy, with high coverage on continuing basis. With impressive achievement for 2 of the targets – 70% of women screened and 90% of women identified with cervical cancer treated – Slovenia could very well become one of the first European countries to reach all 3 targets well in the pathway to elimination. On the other hand, evolution of a cervical cancer free society will take several years in many LMICs which might not comprehensively implement the targeted interventions by 2030.
Challenges in cervical cancer elimination
Lack of political will, national plans for elimination and commitment of resources for cervical cancer prevention in many LMICs is a major challenge. Unaffordable HPV vaccine costs, vaccine hesitancy and vaccine misinformation substantially limit the scope of introduction of elimination programs. Vaccine misinformation, particularly on its safety, unfounded fears on both short- and long-term side effects, vaccine costs and unaffordability for most people and the long latent period for its efficacy to become obvious seem to be the main factors responsible for vaccine hesitancy. Widespread future availability of Indian and other LMIC HPV vaccines will mitigate vaccine costs, access and affordability constraints to a large extent.
Introduction of screening programs require investments in infrastructure and sufficient trained human resources as well as well structured information systems for monitoring and evaluation of the program. Unless these investments are made, it is unrealistic to expect an efficient program reaching all target women above the age of 30 years. WHO strongly recommends HPV testing as the preferred screening method which requires investments in terms of equipment, consumable and trained technicians. The above systematic investments seldom happen in many LMICs.
The unprecedented reallocation of healthcare services necessitated by the COVID-19 pandemic across high-, middle-, and low-income countries, coupled with staff shortages and capacity constraints, is likely to hamper cervical cancer elimination efforts globally with delays in elimination of cervical cancer. Deaths from cancers, including cervical cancer, will increase due to inadequate access to diagnosis and treatment. However, there are valuable lessons to be learnt from COVID-19 control initiatives on the role of advocacy, perseverance and commitment.
Conclusion
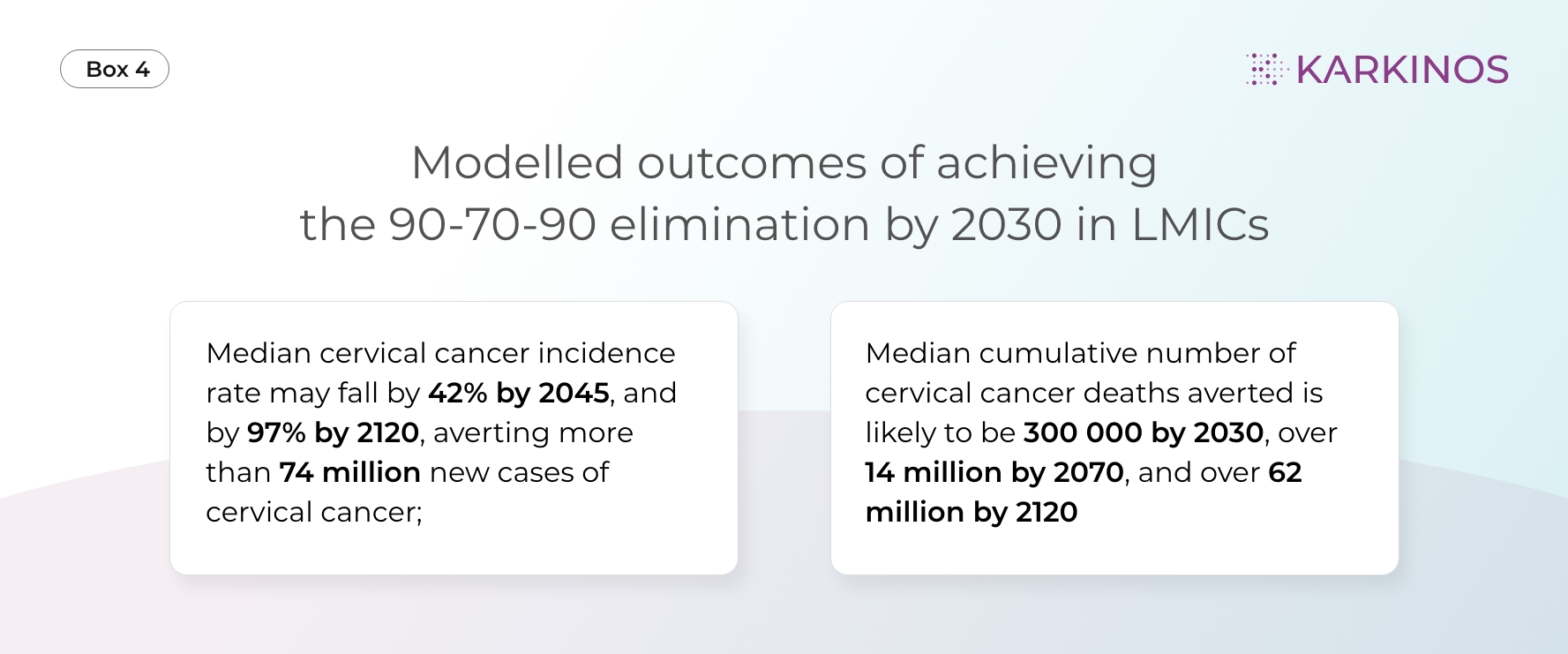
Around the world, one woman dies of cervical cancer every two minutes and without action, cervical cancer cases will increase by 50% in 2030. The modelled outcomes of achieving the 90-70-90 targets by 2030 in LMICs is given in Box 4. Cervical cancer elimination efforts may be equated to steps to eliminate one of the world’s public health failures. Although we have the opportunity, know-how and prevention methods to avoid cervical cancer cases and deaths, these methods have not reached everyone in need. The vision of a world without cervical cancer requires consistent advocacy, improved awareness in all segments of the society, a time bound elimination plan, resource allocation, building infrastructure, augment trained human resources and monitoring and evaluation.
Public-private partnerships can substantially support government initiatives in cervical cancer prevention. Private sector has substantial potential and obligation to contribute to the three- pronged strategy for elimination and it is important to harness this potential.
 About Dr. R. Sankaranarayanan
About Dr. R. Sankaranarayanan